Screening for Sleep Apnea in Railway Workers White Paper
Introduction
On December 1st, 2013, a Metro North passenger train derailed in the Bronx, NY, killing 4, injuring 61 and causing $9 million in property damage. Unfortunately, this accident was not a lone event. According to the Federal Railroad Administration (FRA) Office of Safety Analysis there were 11,233 train incidents including 1,856 accidents and 1,314 derailments in 2015, resulting in 821 lives lost. Among commuter trains, 1,453 passengers were injured and 17 were killed. While the lives lost are the greatest tragedy, the financial costs of these disasters are also massive. Statistics indicate that over the next two decades a subset of trains carrying ethanol or crude oil will derail 10 times per year, resulting in at least $4 billion in damages according to estimates by the Department of Transportation. This figure could be significantly greater if a single railway disaster takes place in a densely populated area like New York City, where damages from such a disaster could reach $11.8 billion. This subset of cost projections only represents a fraction of the total costs from all railway accidents.
In October of 2014, the National Transportation Safety Board (NTSB) concluded that the Metro North derailment was caused by the driver of the train falling asleep due to undiagnosed obstructive sleep apnea (OSA). A five-year study of main-track train collisions by the FRA found that 30% of collisions are related to fatigue.
The Federal Railway Administration (FRA), in conjunction with the Federal Motor Carrier Safety Administration (FMCSA), published a request for comment in the Federal Register in docket numbers MCSA-2015-0419 and FRA-2015-0111 to gather information related to the evaluation of safety sensitive personnel for moderate to severe OSA. In response to this request, the American Sleep Apnea Society has prepared this white paper to address specific questions provided by the agencies.
Given the high prevalence of OSA in railway drivers, the need for screening is urgent. Data suggests that 35% to 62% of railway workers have sleep apnea—a rate that is two to four times greater than the general population. As in the general population, the prevalence increases with risk factors such as age and obesity. A significant amount of these disasters could be prevented by proper screenings that identifies drivers who are likely to be impaired by fatigue.
A comprehensive approach to make our railways safer should include testing for the presence of sleep apnea, evaluation for signs of functional impairment and worker education to prevent and counteract sleepiness during work. Railway workers provide an invaluable service. The lives of others are often dependent on their ability to drive a train while fully functional, at any time, whether at 4 PM or at 4 AM. Since research has demonstrated that self-reported symptoms of sleep apnea in transportation workers are often unreliable, all railway workers in safety sensitive positions should be routinely tested for sleep apnea and impaired function using objective measures.
Those certified to drive a train should:
- Have no sign of sleep apnea on Home Sleep Testing (HST), Polysomnography (PSG), or provide evidence of successful sleep apnea treatment.
- Pass a driving simulator test that mimics nighttime conditions and/or a maintenance of wakefulness test, demonstrating that they do not have a high likelihood of falling asleep when they need to be alert.
Additionally, railway workers should be educated about the risk of driving while sleepy, instructed on proper sleep hygiene, and encouraged to utilize caffeine, rest stops and naps to counteract sleepiness when they are working. A comprehensive screening program in railway drivers should also incorporate safety data collection, so that the benefits of restrictions could be evaluated over time and improved upon. Sleep apnea screening programs can be used to complement other promising technologies such as positive train control (PTC) systems to improve overall railway safety.
Implementation of these recommendations will reduce fatigue related collisions, benefit the health and longevity of railway workers, and reduce their healthcare costs over time. In general, patients with untreated OSA are more likely to have worsening or development of obesity, depression, hypertension, diabetes, stroke, coronary artery disease and cardiac arrhythmias. Their average annual health care costs compared to those without sleep apnea are greater by $1950 to $3899. Therefore, screening of railway workers can efficiently reduce collisions, improve health and result in substantial cost savings.
Key Questions
This white paper attempts to answer the following questions asked by FMCSA and FRA in their request for public comment for proposed rulemaking:
Problem of OSA
- What is the prevalence of moderate-to-severe OSA among the general adult U.S. population? How does this prevalence vary by age?
- What is the prevalence of moderate-to-severe OSA among individuals occupying safety sensitive transportation positions? If it differs from that among the general population, why does it appear to do so? If no existing estimates exist, what methods and information sources can the Agencies use to reliably estimate this prevalence?
- Is there information (studies, data, etc.) available for estimating the future consequences resulting from individuals with OSA occupying safety sensitive transportation positions in the absence of new restrictions? For example, does any organization track the number of historical motor carrier or train accidents caused by OSA? With respect to rail, how would any OSA regulations and the current positive train control system requirements interrelate?
- Which categories of transportation workers with safety sensitive duties should be required to undergo screening for OSA? On what basis did you identify those workers?
Costs and Benefits
- What alternative forms and degrees of restriction could FMCSA and FRA place on the performance of safety-sensitive duties by transportation workers with moderate-to-severe OSA, and how effective would these restrictions be in improving transportation safety? Should any regulations differentiate requirements for patients with moderate, as opposed to severe, OSA?
- What are the potential costs of alternative FMCSA/FRA regulatory actions that would restrict the safety sensitive activities of transportation workers diagnosed with moderate-to-severe OSA? Who would incur those costs? What are the benefits of such actions and who would realize them?
- What are the potential improved health outcomes for individuals occupying safety sensitive transportation positions? Who would receive OSA treatment due to regulations?
- What models or empirical evidence is available to use to estimate potential costs and benefits of alternative restrictions?
- What costs would be imposed on transportation workers with safety sensitive duties by requiring screening, evaluation, and treatment of OSA?
- Are there any private or governmental sources of financial assistance? Would health insurance cover costs for screening and/or treatment of OSA?
Screening Procedures and Diagnostics
- What medical guidelines, other than those the American Academy of Sleep Medicine guidance the Federal Aviation Administration currently uses, are suitable for screening transportation workers with safety sensitive duties that are regulated by FMCSA/FRA for OSA? What level of effectiveness are you seeing with these guidelines?
- What were the safety performance histories of transportation workers with safety sensitive duties who were diagnosed with moderate-to-severe OSA, who are now successfully compliant with treatment before and after their diagnosis?
- When and how frequently should transportation workers with safety sensitive duties be screened for OSA? What methods (laboratory, at-home, split, etc.) of diagnosing OSA are appropriate and why?
- What, if any, restrictions or prohibitions should there be on transportation workers’ safety sensitive duties while they are being evaluated for moderate-to-severe OSA?
- What methods are currently employed for providing training or other informational materials about OSA to transportation workers with safety sensitive duties? How effective are these methods at identifying workers with OSA?
Medical Personnel Qualifications and Restrictions
- What qualifications or credentials are necessary for a medical practitioner who performs OSA screening? What qualifications or credentials are necessary for a medical practitioner who performs the diagnosis and treatment of OSA?
- With respect to FRA, should it use Railroad MEs to perform OSA screening, diagnosis, and treatment?
- Should MEs or Agencies’ other designated medical practitioners impose restrictions on a transportation worker with safety sensitive duties who self-reports experiencing excessive sleepiness while performing safety sensitive duties?
Treatment Effectiveness
- What should be the acceptable criteria for evaluating the effectiveness of prescribed treatments for moderate-to-severe OSA?
- What measures should be used to evaluate whether transportation employees with safety sensitive duties are receiving effective OSA treatment?
The Prevalence of Sleep Apnea
What is the prevalence of moderate-to-severe OSA among the general adult U.S. population?
The best available data suggests that sleep apnea is present in 9% of women and 24% of men ages 30 to 60 in the United States. This comes from the Wisconsin Cohort, a large epidemiological study, which found that self-reported sleepiness was also present in 2% of women and 4% of men leading to a diagnosis of sleep apnea syndrome.1 Wide ranges of OSA prevalence that are reported in some population studies can be attributed to non-uniform study methodologies that defined or measured sleep apnea differently.
How does this prevalence vary by age?
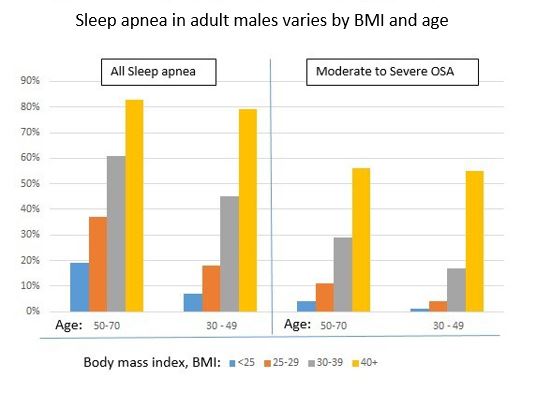
In the United States, a program for monitoring OSA over time isn’t available to provide us with a good estimate of prevalence by age. A model developed using data from the United Kingdom to estimate the prevalence of mild, moderate and severe OSA by age groups in the US2 shows that age and body mass index (BMI) influence the prevalence of all types of OSA. Evidence in railway workers suggests individuals who have a BMI ≥ 25 and are over 37 years old have a higher incidence of OSA.3
Prevalence of sleep apnea in train operators
What is prevalence of moderate-to-severe OSA among individuals occupying safety sensitive transportation positions? If it differs from that among the general population, why does it appear to do so?
The prevalence of sleep apnea in train operators has been shown to be higher than the general population. The reason is likely related to the number of train operators who are male, overweight, smoke, operate in shifts and have other risk factors for OSA.3
Prevalence and risk factors for obstructive sleep apnea syndrome in railway operators was examined in 2 studies3, 4 totaling 1,163 employees. The first study, which examined railway drivers* in Brazil who had an average age of 35.63 years and a mean BMI of 26.74, found that 35% of workers were diagnosed with Obstructive Sleep Apnea Syndrome. This included individuals who had mild apnea (AHI of 5-14) and also had daytime sleepiness that could impair the operation of a train. The majority of workers over 37 years old (51%) had sleep apnea. Since approximately 54.4% of the workers in the study were diagnosed with mild OSA, 25.3% with moderate OSA, and 20.3% with severe OSA, approximately 23% of those over 37 years of age had moderate to severe OSA (assuming an equal distribution across age and BMI in the study).
*The term train “conductors” utilized in the study “Prevalence of and risk factors for obstructive sleep apnea syndrome in Brazilian railroad workers” refers to “drivers.” This is implied in the article and was confirmed by email correspondence with the author, Renata Koyama, on 5/17/16.
Prevalence of OSA in Brazilian railway drivers over 37 or with a BMI of ≥ 25
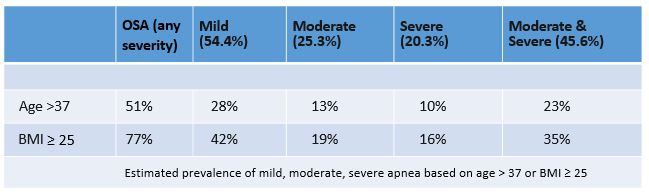
The second study examined railway drivers in Greece and found OSA in 62% of workers whose average age and BMI was 47 years and 28.7, respectively. Similar to the Brazil railway drivers, where 23% were found to have moderate to severe apnea, 22% of the Greek railway drivers had moderate to severe apnea.4
Data on transportation workers in the US show similar descriptive statistics to the railway workers in Greece. For example, US transportation workers have an average BMI of 28.5 5 and an average age of 44.6,6 demographics that are strikingly similar to the cohort of Greek railway drivers (BMI of 28.7 and average age of 47). Generalization of these studies might be made to a US group of railroad workers, in lieu of actual OSA prevalence data from railway workers in the United States.
Consequences and Risk
Is there information (studies, data, etc.) available for estimating the future consequences resulting from individuals with OSA occupying safety sensitive transportation positions in the absence of new restrictions?
According to the FRA Office of Safety Analysis, there were 11,233 train incidents including 1,856 accidents and 1,314 derailments in 2015, resulting in 821 lives lost. Among commuter trains, 1,453 passengers were injured and 17 were killed. The FRA has identified human factors to be the biggest problem, responsible as a primary cause 39% of the time.7 The majority of human factors are likely to be fatigue related, based on a five-year study of main-track train collisions by the FRA which found 30 percent of collisions to be related to fatigue. 8 Of note, the term “fatigue” is routinely used by federal agencies such as the NTSB to describe what sleep specialists call excessive “sleepiness.” 9
Financial impact
The greatest cost of railway accidents are the lives lost, but the direct and indirect financial costs of railway accidents are projected to be in the billions. The Department of Transportation’s Pipeline and Hazardous Materials Safety Administration, looking only at a subset of trains carrying ethanol or crude oil, project that these trains will derail 10 times per year on average over the next two decades, resulting in $4 billion in damages.10 These projections rely on data from prior catastrophes including the Lac-Mégantic accident in the Canadian province of Quebec, which killed 46 individuals and had costs estimated around $2.7 billion. Some make the case that these projections could be severely underestimated.11 For example, railroad companies have frequently cited a 2006 damage assessment report by the American Academy of Actuaries for the President’s Working Group on Financial Markets to estimate damages of an oil tanker explosion in a more densely populated area. Using the closest analogy, a truck bomb explosion would result in damages of $3 billion near Des Moines, $8.8 billion in San Francisco, and $11.8 billion near New York City. Despite debate over estimates, these cost projections only represents a fraction of the costs of the total number of railway accidents.
The Metro-North passenger train derailment
On December 1st, 2013 shortly after 7:19 AM, a passenger train derailed in the Bronx, NY, killing 4, injuring 61 and causing $9 million in property damage.12 As of December 2015 an additional $38 million dollars in lawsuits had been settled.13
Impact of lost service on gross domestic product (GDP)
A single accident might also indirectly impact the contribution to GDP from workers traveling on a route that is temporarily disabled. An article in Fortune Magazine published after an Amtrak passenger derailment on May 13, 2015 cited company officials who estimated that a single day of lost service could cost $100 million to affected businesses and consumers. 14
Does any organization track the number of historical motor carrier or train accidents caused by OSA?
The NTSB issues accident reports following the investigation of train accidents in the United States. This data often explores prior medical records, often reporting on accidents that are caused by OSA. However, this data may underestimate OSA incidence due to cases of undiagnosed OSA.
Making Our Railways Safer
Given the high costs of railway disasters, applying a multimodal approach towards preventing accidents is prudent. A comprehensive approach to make our railways safer should include testing for the presence of sleep apnea, evaluation for signs of functional impairment, and worker education to prevent and counteract sleepiness during work.
Railway workers provide an invaluable service. Their own lives as well as the lives of others are often dependent on their ability to drive a train while fully functional, at any time.
Several technologies such as Positive Train Control (PTC) Systems have been developed and can provide one mechanism of improving safety. Still, a great deal of accidents are attributed to fatigue. Given the high prevalence of sleep apnea in railway drivers, the need for a comprehensive approach to screening is urgent.
With respect to rail, how would any OSA regulations and the current PTC requirements interrelate?
PTC systems can act as safety measures to improve overall railway safety. These devices can increase train safety through automation, such as technology that slow trains moving too fast around a curved section of rail. Despite this technology, it is of utmost importance to ensure the highest level of human performance because railway workers play an essential role in the safety of trains.
Objective sleep apnea testing for all workers
Which categories of transportation workers with safety sensitive duties should be required to undergo screening for OSA? On what basis did you identify those workers?
All transportation workers with safety sensitive duties should undergo sleep testing. The unique risks posed by railway workers in safety sensitive positions, especially drivers, as well as the great human and financial costs involved in each wreck justify screening every worker. However, unlike traditional assessments which rely strongly on a patient’s self-report of symptoms, screening transportation workers should rely strongly on objective testing such as polysomnography, home sleep testing, maintenance of wakefulness testing and driving simulators.
Research has repeatedly demonstrated an inability for medical examiners to reliably elicit symptoms from transportation workers by traditional history (i.e., questions and answers). Establishing screening programs in these workers, therefore, needs to rely upon objective testing. This would provide for the safest and most prudent approach. It would also be the simplest to implement. Every worker with a need for sustained attention (i.e., drivers) should undergo diagnostic testing for sleep apnea with home sleep testing or polysomnography. These tests can usually identify the presence of latent sleep apnea, which is undiagnosed in 40% to 80% of individuals who have the disease. In certain circumstances a polysomnogram, which is more sensitive for the detection of sleep apnea, may be the preferred test.
The American Academy of Sleep Medicine (AASM) guidelines of 200915 are relied upon by the Federal Aviation Administration for their guide for medical examiners to screen for sleep apnea. While the AASM guidelines do consider “driving populations” as high-risk populations, those guidelines were geared towards an evaluation of the general population and therefore were not specifically devised for transportation workers.
Traditional sleep apnea evaluations that rely on subjective symptom reporting are unreliable in evaluating transportation workers. In clinical practice, the most commonly reported symptoms of sleep apnea include snoring and excessive sleepiness. Sleepiness is often self-reported or elicited and quantified through the use of surveys, such as the Epworth Sleepiness Scale (ESS). On average, individuals who are excessively sleepy have an ESS score of 10 or above and those with sleep apnea have an average ESS score of about 13. However, when transportation workers, such as commercial drivers, are surveyed at driver certification exams, they report very low ESS scores, that are, in fact, lower than the general community. Some drivers with OSA evidence “deception,” reporting even lower ESS scores than drivers without OSA .16 Similar observations about sleepiness were made in the cohort of Greek railway drivers (cited above) who had moderate to severe sleep apnea, but reported normal ESS scores. The drivers with the most severe cases of sleep apnea (mean AHI = 68) reported even lower ESS scores than the drivers with moderate apnea.4 Therefore, in lieu of using an ESS and other subjective measurements or self-reports to assess sleepiness due to the limitations mentioned above, the Maintenance of Wakefulness test (MWT) 17 or, possibly, a railway driving simulator, could be used for greater accuracy.
Maintenance of wakefulness testing
What alternative forms and degrees of restriction could FMCSA and FRA place on the performance of safety-sensitive duties by transportation workers with moderate-to-severe OSA?
The MWT is the gold standard, objective, valid and reliable measure of excessive daytime sleepiness in clinical practice, which tests the ability of a subject to maintain wakefulness while engaging in a quiet or boring situation (i.e., sitting on a comfortable chair in a semi-dark room).18 The MWT can discriminate between sleepy and alert drivers with OSA. Research has found an association between drivers with OSA who are “sleepy” on MWT and those who perform poorly on driving simulators. 19
The sleepier a driver is, the more likely their performance will suffer. In addition to sleep apnea, risk factors for fatigue among workers include uncertain shift times, long commutes, sub-optimal terminal sleeping conditions, and insufficient sleep before a night shift. Similar to reports from other shift workers, train drivers beginning their shift between 10 PM and 4 AM have reported sleeping insufficiently (fewer than 6 hours a day on average), which leaves them sleep deprived. 20 A relationship also exists between age and sleepiness—older patients with OSA are more likely to exhibit excessive sleepiness on an MWT. 21
While many individuals with OSA or those who are sleep restricted are consistently impaired on driving simulators, a small subset of these individuals may routinely function normally on driving simulation. This suggests that other factors may play a role in determining individuals who are most likely to be impaired by OSA.19 Since the response to sleep disruption cannot be solely accounted for by the presence of OSA or its severity, other objective testing (in addition to the diagnosis and treatment of OSA in railway workers) is needed to establish that railway workers are fit to drive.
Psychomotor vigilance testing
The Psychomotor Vigilance Test (PVT) is a sustained attention psychometric test that has not yet been established to predict poor driving performance. The PVT measures the reaction time of a subject’s response to visual stimuli. In sleep research it has been used to identify drowsiness secondary to disturbed or insufficient sleep. The advantage of this test is that it can generally be performed in less than 10 minutes and provide immediate feedback regarding attention levels. However, we could not find any data during our review of related literature establishing that poor performance on the PVT can be used to predict impaired driving. Further research is required to identify whether PVT or another short duration psychometric test might be utilized to identify drivers who are more likely to be impaired as a result of sleep deprivation or OSA.
Driving simulators
Railway driving simulators or railway driving data analysis may offer the best possible tool to identify drivers who are impaired by OSA or other causes. While MWT indirectly gauges risk by identifying an individual’s ability to stay awake, driving simulation pinpoints performance that is impaired even when a driver is “awake.” Research looking at MWT to evaluate its ability to assess driver impairment has frequently compared MWT results to driving simulator performance. 19, 22-26 Most of these studies have looked at the driving of an automobile, measuring steering deviation, lane deviation and crashes. In some studies, simulators have been set up to mimic nighttime driving.19 Simulators for railway driving track features such as speed approach of the crossing, head movements, and stopping compliance.27 Furthermore, some of the research that establishes that MWT could be used to assess driving ability in untreated patients with OSA analyzes actual driving session data.26 One of the best tools to identify drivers who are fit-for-duty or to flag drivers who have an underlying sleep disorder may be to utilize current railway simulators to mimic nighttime driving situations, which is when most railway accidents take place. Analyzing real time driver data to track similar safety and performance metrics might also be an effective means of establishing drivers that are fit-for-duty or flagging drivers that are not.
Tracking treatment compliance and efficacy
All individuals who are diagnosed with mild, moderate or severe OSA and treated with continuous positive airway pressure (CPAP) should demonstrate that they are adherent to treatment. This is accomplished by CPAP devices that track compliance data as well as the efficacy of treatment. Individuals who undergo treatment with an oral appliance must undergo a sleep study with the appliance in place to demonstrate that their device is effective to relieve the apnea. If effective, it is also important to ensure compliance with treatment. Recently developed technology allows compliance data to be tracked in oral appliances.
An important part of fatigue management is ensuring that all operators are ready to perform and fit for duty. Treating OSA may relieve the root cause of sleepiness in a driver. However, the only way to ensure that a driver is not functionally impaired is to test their ability to stay awake and perform. Therefore, restrictions should focus on ensuring that those with OSA are treated and, perhaps equally important, that they are able to perform without the adverse effects of sleepiness.
All individuals diagnosed with OSA, even those who deny any sleepiness and those who are treated successfully with CPAP or an oral appliance, should routinely demonstrate through an approved driving simulation or MWT that they are fit to drive in situations that require sustained attention.
How effective would these restrictions be in improving transportation safety?
Data from driving simulators and crash data have demonstrated that driving capabilities return in patients with OSA that are treated with CPAP. In motor vehicles, baseline performance has been shown to return within a matter of days. 28, 29 It is advised that a screening program in railway drivers should also collect and continue to monitor safety data for continuous evaluation, quality control and program improvement.
The difference between mild, moderate and severe apnea
Should regulations differentiate requirements for patients with moderate, as opposed to severe, OSA?
Excessive sleepiness can be observed at any level of sleep apnea and is not limited to moderate-to-severe OSA. The most commonly utilized parameter to categorize the severity of sleep apnea is the apnea-hypopnea-index or the AHI, which reports the rate of respiratory events known as apneas or hypopneas during sleep. An AHI of < 5 is normal, 5-14 is considered to be mild sleep apnea, 15-29 is considered moderate, and 30 or more is considered to be severe OSA. While an AHI of 20 or greater has been shown as an independent risk factor for excessive sleepiness in some studies,30 numerous studies have shown excessive sleepiness in patients with mild forms of OSA. For example, in the study of rail workers from Brazil mentioned above, 54.4% of those with OSA had a mild form that was associated with excessive sleepiness. In fact, excessive sleepiness may be present in patients with a normal AHI (AHI <5) who could be diagnosed utilizing an alternative, less frequently utilized criteria for OSA diagnosis known as the respiratory disturbance index (RDI).* Like the AHI, this index reports the rate of apneas and hypopneas, together with another parameter known as respiratory effort related arousals (RERAs). Furthermore, the use of HST, which is advocated for herein, reduces the accuracy of discriminating between mild and moderate sleep apnea or between moderate to severe apnea, as it tends to underestimate the total severity of sleep apnea. Therefore, limiting regulations to those with moderate or severe OSA could leave a substantial portion of patients who have excessive sleepiness undetected even though their AHI might only qualify them as having “mild” sleep apnea (AHI <15).
*The definition of RDI used above includes RERAs and can be detected by polysomnography and not through HST. Some organizations may refer to RDI and AHI, synonymously, omitting RERAs.
Costs & Benefits of Apnea Diagnosis & Treatment
What are the potential costs of alternative FMCSA FRA regulatory actions that would restrict the safety sensitive activities of transportation workers diagnosed with moderate-to-severe OSA?
Medical costs
The main costs relate to evaluation, diagnosis and treatment of sleep apnea. Costs may vary, depending upon providers, payors, regions and the types of tests being implemented. However, approximate costs can be estimated by looking at Medicare physician reimbursement fees.31 According to these figures, the cost of diagnosis would range from $170 for an HST to $796 for a negative HST followed by a confirmatory PSG. CPAP titration studies would cost about $658. A CPAP machine and supplies for 1-year costs about $1,000.32 An MWT, which is used to identify subsets of excessively sleepy individuals, costs about $424. However, there is great variation in the contracted rates of providers and insurance companies, providing an opportunity to reduce overall costs for high-volume screening programs.
Costs related to treatment
The average annual cost for treatment for an individual found to have sleep apnea, including physician follow up, additional supplies, and an additional CPAP titration study every 5 years is estimated to cost around $1,200/year.32 Alternative treatments for OSA, such as an oral appliance or surgery, would cost around $1,500 and $10,000, respectively. Furthermore, costs can be increased by failure rates of modalities of treatment then leading to another modality being tried.
The majority of costs are generally highest in the first year. Average costs can be lowered by starting treatment with CPAP in all patients, advancing to an oral appliance only after therapy failure with CPAP, and only utilizing surgery as a last resort for treatment.
Who would incur those costs? What are the benefits of such actions and who would realize them?
The costs related to evaluation, diagnosis, treatment and continued management of sleep apnea are usually paid for by an individual’s health insurance. It is less clear if insurance companies would cover the MWT testing. While this is the “gold standard” for evaluation of the ability to stay awake, it is not routinely implemented in the evaluation of patients with sleep apnea, as the majority of patients do not work in sensitive positions such as driving a train. In general, all reimbursement would be subject to variability in individual plans, deductibles, co-payments and related individual/family healthcare utilization. The benefits of treating sleep apnea are well described and elaborated upon below. While healthcare costs might increase in the short-term for patients diagnosed with the disease, long-term health care costs of individuals treated with sleep apnea are expected to decrease over time. In general, patients with untreated OSA incur additional costs of $1950 to $3899 per year in comparison to those who do not have OSA.33 Therefore, the health and financial benefits would accrue to the individual, employer and to the public.
Health benefits of treatment
What are the potential improved health outcomes for individuals occupying safety sensitive transportation positions and would receive OSA treatment due to regulations?
There are well established relationships between untreated sleep apnea and the development or worsening of obesity, depression, hypertension, diabetes, stroke, coronary artery disease, and cardiac arrhythmia. Individuals with untreated sleep apnea have a reduced quality of life and a shorter life span.33 Treating OSA successfully mitigates or reverses most of these risks.
What models or empirical evidence is available to use to estimate potential costs and benefits of alternative restrictions?
Several of the tests suggested in this paper might be considered “alternatives” to the traditional evaluation of sleep apnea, such as the MWT, for which we have provided cost data (see “Medical Cost” above) that is available from the Centers for Medicare and Medicaid Services.
Paying for apnea
What costs would be imposed on transportation workers with safety sensitive duties by requiring screening, evaluation, and treatment of OSA?
In general, screening, evaluation, and treatment of OSA is paid for by health insurance companies. However, transportation workers or their employers would be responsible for deductibles, co-payments and uncovered screening, evaluation and treatment of OSA. If patients do not report snoring or excessive sleepiness, coverage for a sleep test from an insurance company could be denied. In the general population, there is no specific incentive to under-report symptoms. However, as discussed above, under-reporting is common in transportation workers. This could contribute to cost of testing being shifted towards the workers and employers in many cases.
Are there any private or governmental sources of financial assistance? Would health insurance cover costs for screening and/or treatment of OSA?
As discussed, reimbursement varies based on the insurer. It is likely that all screening and treatment of OSA would be paid for in the cases of transportation workers. It may also be a shared cost or one that might need special negotiation if the decision is made to test all workers rather than only testing individuals who meet the sleep testing criteria established for the general population.
Screening and Testing for OSA
Prior guidelines for screening workers
What medical guidelines other than the AASM FAA currently uses are suitable for screening transportation workers with safety sensitive duties that are regulated by FMCSA FRA for OSA?
Guidelines of the AASM are not appropriate for the “screening” of transportation workers, and implementation for railway workers requires modification. Any screening needs to account for the expected lack of self-reported symptoms in transportation workers. The simplest way to do this would be to have all workers undergo home sleep testing or a PSG, and either an MWT or a driving simulator.
Risk stratification utilizing age, body mass index (BMI), neck circumference or the presence of medical comorbidities including diabetes, hypertension, heart disease or depression may be appropriate to identify the frequency of evaluation. Risk for OSA should not be ruled out by self-reports of being alert, not being excessively sleepy, or denying other symptoms (i.e., snoring).
What level of effectiveness are you seeing with these guidelines?
Union Pacific Health System, the health care provider for 20,000 Union Pacific (UP) railroad workers, began an effort to screen their workforce for sleep apnea about ten years ago. The “Complete Sleep Program” spent over $579,730 in their first year. The program began to see fiscal gains by the second year, when they saved $422,652, mostly from decreased hospital admissions. By the fourth year the company saw their health care cost decrease by 28%. The company reported saving $4.9 million by the seventh year of the program.34
What were the safety performance histories of transportation workers with safety sensitive duties who were diagnosed with moderate-to-severe OSA, who are now successfully compliant with treatment before and after their diagnosis?
While we have no specific records available to us to review, as mentioned earlier, data from driving simulators and crash data have demonstrated that driving capabilities return to baseline in patients with OSA treated with CPAP in a matter of days. 28, 29 Therefore, it is reasonable to expect that the risk posed by untreated OSA would be mitigated through treatment in transportation workers.
Frequency of testing workers
When and how frequently should transportation workers with safety sensitive duties be screened for OSA?
Transportation workers should be screened for OSA with a sleep study at least once every 5 years. This frequency should be informed by the likelihood of developing sleep apnea over time. Several longitudinal studies have found that a significant number of patients will develop OSA within 5 years of a negative sleep study. The Cleveland Family Study found that 7.5 % of participants developed at least moderate OSA (AHI>15) and 16% developed an AHI > 10 within 5 years of a negative sleep study. The Sleep Heart Health Study demonstrated that the 5-year incidence of at least moderate OSA was higher in men, with 11.1% of men developing sleep apnea.1
It would be prudent to look at other areas of public health screening to inform the frequency of testing. For example, both cervical cancer* and HIV testing consider risk factors to determine screening intervals. Individuals with various risk factors are much more likely to have OSA. In these populations, detecting sleep apnea may not be a question of “if” but “when.” Therefore, increased frequency of screening is prudent. In patients with an Age > 37 or a BMI ≥ 25, a sleep study every 2 years might be performed. In patients with an Age > 50, a BMI >30, or a history of congestive heart failure, atrial fibrillation, hypertension, diabetes, stroke, or chronic obstructive pulmonary disease (COPD), an annual sleep study might be prudent. The absence of sleep apnea on 3 consecutive tests*, might be utilized to reduce the frequency of testing in a higher risk individual. For example, decreasing the interval of sleep apnea testing from annually to once every 2 years.
Furthermore, annual driving certification is recommended for all workers where workers can be certified after demonstrating that they have no sign of sleep apnea on a prior HST or PSG. If they have been diagnosed with sleep apnea, they should provide evidence of treatment compliance and successful sleep apnea treatment. Additionally, prior to certification all drivers should be subject to annual driving simulator testing that mimics nighttime conditions and/or a maintenance of wakefulness test, demonstrating that they do not have a high likelihood of falling asleep when they need to be alert. Failure of these tests might trigger a repeat sleep study or an evaluation for an alternative cause of impaired performance.
* Three consecutively negative pap smears are commonly used to reduce interval frequency in cervical cancer screening.
Types of overnight sleep tests for identifying sleep apnea
What methods (laboratory, at-home, split, etc.) of diagnosing OSA are appropriate and why?
Home sleep testing (HST) can diagnose most cases of moderate to severe OSA. It is easier to implement on a wide scale than PSG. However, HST can underestimate the severity of sleep apnea leading to false negative results, characterizing severe apnea as moderate, or moderate sleep apnea as mild. There is also some concern that individuals could “cheat” the test by having someone else wear the device. It is unclear that this would happen. However, the risk could be mitigated by repeating a laboratory-based PSG in individuals who have a negative HST. This is often the standard of care due to the false negative rate inherent in HST. Educating individuals about the fact that a negative home study will result in another in-lab PSG study would likely act as a deterrent to this type of behavior. Alternatively, technologies could be employed to ensure that a specific individual is using the HST, although we are unaware if any commercially available HSTs have this capability. The implementation of railway driving simulator testing or MWT adds another incentive for individuals not to “cheat” a home sleep test, as it could lead to failing the subsequent MWT or simulator.
Laboratory based PSG offers the most accurate method to diagnose OSA. It is the gold standard for evaluation. The risk of “cheating” the test is mitigated by having to present to a sleep lab where a requirement of showing identification and other security measures can be taken.
Individuals with a “positive” PSG or HST, showing evidence of sleep apnea, generally undergo an overnight in-lab continuous positive airway pressure (CPAP) titration study, also known as a PSG titration study. This study takes place in a sleep laboratory and is monitored by a sleep technologist who follows a protocol for increasing the pressure to a level sufficient to eliminate OSA using CPAP during sleep.
Split-night testing refers to adding a CPAP titration to an in-lab diagnostic PSG study when severe apnea is identified in the beginning of a sleep study. It has the advantage of decreasing the need for 2 nights in a sleep lab to only 1 night of sleep testing, resulting in initiating treatment earlier. If severe apnea is not detected in the first several hours of the night, the study proceeds as a routine diagnostic PSG and therefore not every “split” study gets divided.
Restricting activities of workers during evaluation
What, if any, restrictions or prohibitions should there be on a transportation workers safety sensitive duties while they are being evaluated for moderate-to-severe OSA?
Transportation workers should not be certified to drive a train unless they:
- Have no sign of sleep apnea on Home Sleep Testing, Polysomnography (PSG) or if they provide evidence of successful sleep apnea treatment.
- Pass a driving simulator test that mimics nighttime conditions and/or a maintenance of wakefulness test, demonstrating that they do not have a high likelihood of falling asleep when they need to be alert.
Utilizing education to improve outcomes
What methods are currently employed for providing training or other informational materials about OSA to transportation workers with safety sensitive duties? How effective are these methods at identifying workers with OSA?
Education can enhance recognition of sleep disorders by the population and healthcare providers. A community based educational program was shown to increase referrals for sleep testing by 8 times over a two year period.35 Similarly, education can also improve compliance and efficacy of sleep apnea treatment.36 While data on educational interventions specific to sleep apnea is limited, previous public health campaigns in other areas (i.e. blood pressure screening, Sudden Infant Death Syndrome (SIDS) prevention, anti-smoking) have demonstrated an ability to reduce risky behavior.37 Therefore, patients with sleep apnea should be educated about the risk of driving while sleepy, instructed on proper sleep hygiene, and encouraged to utilize caffeine, rest stops and naps to counteract sleepiness.38
Medical Personnel Qualifications & Restrictions
What qualifications or credentials are necessary for a medical practitioner who performs OSA screening? What qualifications or credentials are necessary for a medical practitioner who performs the diagnosis and treatment of OSA?
The qualifications required depend upon the complexity that is involved in the eventual screening process. While it is always preferable to have sleep medicine specialists treating patients with sleep apnea, it is not always practical or necessary. A certification course including an educational and testing component could be provided to medical practitioners in person or via the internet to ensure that they are up to date with the guidelines instituted by the organization for screening. By implementing a simple screening process where all employees in sensitive positions undergo a sleep study, the results of the sleep study and its recommendations can be reviewed and implemented by any health care practitioner. They can also order a follow up CPAP titration study and CPAP equipment. Counseling and chronic management of patients on CPAP, especially those who have problems complying with CPAP treatment, could be performed by sleep specialists, but could be learned by any medical practitioners. These medical practitioners could elect to refer select patients to a specialist as is customary in routine medical practice.
With respect to FRA should it use Railroad MEs to perform OSA screening, diagnosis, and treatment?
Railroad Medical Examiners should incorporate screening for OSA into their health exams. To the extent that they are available to do so, and in combination with other providers and specialists, railroad MEs can help implement large scale OSA screenings.
Should MEs or other Agencies’ designated medical practitioners impose restrictions on a transportation worker with safety sensitive duties who self-reports experiencing excessive sleepiness while performing safety sensitive duties?
Evidence demonstrates that transportation workers are unlikely to self-report symptoms of OSA. Requiring medical practitioners to impose restrictions on those who do report excessive sleepiness might further reduce the likelihood that employees will seek medical attention.38 It is preferred that MEs play a role in certifying all drivers by relying on objective evidence of not being sleepy such as passing an MWT or a driving simulation. For patients that remain sleepy or unable to maintain alertness, treatment with modafinil, armodafinil, stimulants or other interventions should be considered. While medical examiners should not be imposing restrictions, drivers who are objectively sleepy should not be certified to drive.
What should be the acceptable criteria for evaluating the effectiveness of prescribed treatments for moderate-to-severe OSA?
Many CPAP devices can track user compliance and provide a report related to the effectiveness of treatment such as a 30-day or 90-day AHI that can demonstrate treatment efficacy when the machine is being used. While Medicare requires that individuals use CPAP 4 hours a night for 70% of nights, there is a dose-dependent relationship between the amount of time CPAP is being used and its effectiveness with respect to the symptoms of sleep apnea. Tracking compliance and therapeutic data should also be a standard applied for individuals who are wearing an oral appliance. The oral appliance should have the capabilities to track user compliance and a subsequent MWT or driving simulation should provide evidence that the individual is not excessively sleepy.
What measures should be used to evaluate whether transportation employees with safety sensitive duties are receiving effective OSA treatment?
Effectiveness of OSA treatment, from a railroad safety perspective, should be gauged based on the effect it has related to sleepiness. Therefore, an individual should be compliant with treatment but also able to pass an MWT or driving simulation without exerting evidence that they are excessively sleepy.
Conclusion
All railway workers in safety sensitive positions should be routinely tested for sleep apnea and impaired function using objective measures. Sleep apnea in railway drivers represents a potentially reversible cause of a large number of railway incidents. Screening for sleep apnea needs to be comprehensive, focusing on identification of sleep apnea as well as an evaluation for signs of functional impairment. Education and other technological advances can also help support improving railway safety. Railway workers bear an awesome responsibility and many lives depend upon their ability to drive a train while fully functional, at any time, whether it be at 4 PM or at 4 AM. Research has demonstrated that self-reported symptoms of sleep apnea in transportation workers are often unreliable.
Those certified to drive a train should:
- Have no sign of sleep apnea on Home Sleep Testing, Polysomnography (PSG) or provide evidence of successful sleep apnea treatment.
- Pass a driving simulator test that mimics nighttime conditions and/or a maintenance of wakefulness test, demonstrating that they do not have a high likelihood of falling asleep when they need to be alert.
Those found to have sleep apnea need to be monitored to ensure compliance with treatment. Individuals without apnea should also be able to demonstrate that they are able to drive and maintain their level of alertness. Additionally, they should be tested at regular intervals to identify apnea that can develop at any time.
Implementation of these recommendations can be accomplished in a cost-effective manner that will reduce fatigue related collisions, benefit the health and longevity of railway workers and reduce healthcare costs over time.
Acknowledgements
The American Sleep Apnea Society and Dr. Michael Morgenstern would like to thank our volunteers Rachel Schottenfeld and Kimberly Thomas for their contribution to this paper. We are also extremely grateful for the review and guidance of Dr. Harly Greenberg, Chief of the Division of Pulmonary, Critical Care and Sleep Medicine and Medical Director of the Sleep Disorders Center at Northwell Health and Professor of Medicine at the Hofstra Northwell School of Medicine.
Health Information Disclaimer:
The American Sleep Apnea Society has provided this white paper for informational purposes only. The materials contained here are not intended to be used for the diagnosis or treatment of a health problem or as a substitute for professional medical advice, diagnosis or treatment from a licensed medical professional. Never disregard professional medical advice or delay in seeking treatment because of something you have read here. The American Sleep Apnea Society assumes no responsibility for any discrepancies or errors contained in these resources.
References
- Lee W, Nagubadi S, Kryger MH, Mokhlesi B. Epidemiology of Obstructive Sleep Apnea: a Population-based Perspective. Expert review of respiratory medicine. 2008;2(3):349-364. doi:10.1586/17476348.2.3.349. (Link)
- Peppard, Paul E., et al. “Increased prevalence of sleep-disordered breathing in adults.” American journal of epidemiology(2013): kws342. (Link)
- Koyama, Renata G., et al. “Prevalence of and risk factors for obstructive sleep apnea syndrome in Brazilian railroad workers.” Sleep medicine8 (2012): 1028-1032. (Link)
- Nena, Evangelia, et al. “Sleep-disordered breathing and quality of life of railway drivers in Greece.” CHEST Journal1 (2008): 79-86. (Link)
- Luckhaupt, Sara E., et al. “Prevalence of obesity among US workers and associations with occupational factors.” American journal of preventive medicine3 (2014): 237-248. (Link)
- The U.S. Bureau of labor Statistics. (2013).Employed persons by detailed industry and age. Retrieved from BLS.gov (Link)
- The U.S Federal Railroad Administration (2006) The Railroad Fatigue Risk Management Program at the Federal Railroad Administration: Past, Present and Future. Retrieved from https://www.fra.dot.gov/Elib/Document/2944 (Link) Also see: https://www.fra.dot.gov/Elib/Document/1683 (Link)
- Collision Analysis Working Group (CAWG) 65 Main-Track Train Collisions, 1997 through 2002: Review, Analysis, Findings and Recommendations, CAWG Final Report, July 2006 (Link)
- Institute of Medicine. Sleep disorders and sleep deprivation. An unmet public health problem. Washington, DC: National Academy of Sciences; 2006.
- Department of Transportation Pipeline and Hazardous Materials Safety Administration. Draft Regulatory Impact Analysis. Hazardous Materials: Enhanced Tank Car Standards and Operational Controls for High-Hazard Flammable Trains; Notice of Proposed Rulemaking. July 2014. (Link)
- Sightline Institute. What do oil train explosions cost? Retrieved from http://www.sightline.org/2014/12/18/what-do-oil-train-explosions-cost (Link)
- National Transportation Safety Board Railroad Accident Brief. Metro-North Railroad Derailment. October 2014. Retrieved from http://www.ntsb.gov/investigations/AccidentReports/Reports/RAB1412.pdf (Link)
- USA Today. Commuter rail accidents cost N.Y. $38M, still climbing. October 2015. (Link)
- Fortune Magazine. What’s the economic impact of the Amtrak crash? May 2015. (Link)
- Epstein, Lawrence J., et al. “Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults.” J Clin Sleep Med3 (2009): 263-276. (Link)
- Kales, Stefanos N., and Madeleine G. Straubel. “Obstructive sleep apnea in North American commercial drivers.” Industrial health1 (2014): 13-24. (Link)
- Johns, Murray W. “Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the Epworth sleepiness scale: failure of the MSLT as a gold standard.” Journal of sleep research1 (2000): 5-11. (Link)
- Pizza, Fabio, et al. “Daytime sleepiness and driving performance in patients with obstructive sleep apnea: comparison of the MSLT, the MWT, and a simulated driving task.” Sleep3 (2009): 382. (Link)
- Vakulin, Andrew, et al. “Individual variability and predictors of driving simulator impairment in patients with obstructive sleep apnea.” J Clin Sleep Med6 (2014): 647-55. (Link)
- Dorrian, Jillian, et al. “Simulated train driving: Fatigue, self-awareness and cognitive disengagement.” Applied ergonomics2 (2007): 155-166. (Link)
- Sagaspe, Patricia, et al. “Maintenance of wakefulness test as a predictor of driving performance in patients with untreated obstructive sleep apnea.”SLEEP 3 (2007): 327. (Link)
- George CF, Boudreau AC, Smiley A. Simulated driving performance in patients with obstructive sleep apnea. Am J Respir Crit Care Med 1996;154:175-81.
- Pizza F, Contardi S, Mondini S, Trentin L, Cirignotta F. Daytime sleepiness and driving performance in patients with obstructive sleep apnea: comparison of the MSLT, the MWT, and a simulated driving task. Sleep 2009;32:382-91.
- Sagaspe P, Taillard J, Chaumet G, et al. Maintenance of wakefulness test as a predictor of driving performance in patients with untreated obstructive sleep apnea. Sleep 2007;30:327-30.
- Philip P, Chaufton C, Taillard J, et al. Maintenance of Wakefulness Test scores and driving performance in sleep disorder patients and controls. Int J Psychophysiol 2013;89:195-202.
- Philip P, Sagaspe P, Taillard J, et al. Maintenance of Wakefulness test, obstructive sleep apnea syndrome, and driving risk. Ann Neurol 2008;64:410-6.
- Larue, Grégoire S., et al. “Driver’s behavioural changes with new intelligent transport system interventions at railway level crossings—A driving simulator study.”Accident Analysis & Prevention 81 (2015): 74-85. (Link)
- George CF. Reduction in motor vehicle collisions following treatment of sleep apnoea with nasal
Thorax. 2001;56:508-512. - Turkington PM, Sircar M, Saralaya D, Elliott MW. Time course of changes in driving simulator
performance with and without treatment in patients with sleep apnoea hypopnoea syndrome. Thorax. 2004;59:56-59. - Pack, Allan I., et al. “Risk factors for excessive sleepiness in older adults.”Annals of neurology6 (2006): 893-904.
- The American Academy of Sleep Medicine. Sleep Services Payment Comparison 2014 National Payment vs. 2015 National Payment. (Link)
- McKinsey& Company. The price of fatigue: The surprising economic costs of unmanaged sleep apnea. 2010. (Link).
- Knauert, Melissa, et al. “Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome.” World Journal of Otorhinolaryngology-Head and Neck Surgery1 (2015): 17-27. (Link)
- com. Cost savings viewed as critical benefit of combating sleep apnea. October 2012. (Link)
- Ball, Eric M., et al. “Diagnosis and treatment of sleep apnea within the community: the Walla Walla project.” Archives of Internal Medicine4 (1997): 419-424. (Link)
- Ballard, Robert D., Peter C. Gay, and Patrick J. Strollo. “Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure.” J Clin Sleep Med7 (2007): 706-712. (Link)
- Altevogt, Bruce M., and Harvey R. Colten, eds. Sleep Disorders and Sleep Deprivation:: An Unmet Public Health Problem. National Academies Press, 2006. (Link)
- Findley L. The threat of mandatory reporting to a driver’s license agency discourages sleepy drivers from being evaluated for sleep apnea. Sleep. 2002;25:A224.
Photo Credits: Wikipedia.org /Grand_union /High-speed_rail_in_the_United_States /Conductor_(rail)